A case series study- massage prescription for insomnia

I have noticed that a significant number of my clients are experiencing challenges with their sleep. To address this issue, I undertook a small-scale study involving three participants to explore potential treatment guidelines for massage therapists to utilize when working with individuals suffering from insomnia. Despite the limitations of this study, it serves as a foundational step towards the development of a tailored approach to massage therapy for those grappling with sleep disturbances. Looking ahead, my aspiration is to witness the integration of massage therapy as a prescribed solution for addressing sleep-related difficulties.
Why?
Previous research has extensively covered insomnia, including its effects and available treatments. However, this study aimed to examine the impact of a commonly used Swedish massage therapy on individuals who have insomnia and high blood pressure over eight weeks. The study will investigate whether Swedish massage sessions can effectively alleviate symptoms of insomnia and provide empirical evidence for individuals to use massage as an effective treatment.
Introduction of some the Facts
Insomnia is a sleep disorder that affects a significant percentage of people worldwide. The severity of the disorder can vary depending on the definition of chronic insomnia, but generally, it is characterized by difficulty falling asleep, interrupted sleep, nonrestorative sleep, and early morning awakenings occurring three or more times a week for at least a month.
Up to one-third of the general population experiences at least one clinical insomnia symptom, including daytime consequences, sleep dissatisfaction, and insomnia diagnoses. Of those affected, 15-20% report experiencing daytime impairment, while 5-10% meet the standardized diagnostic criteria.
According to a study, 13% of New Zealand’s population aged between 20-59 years experiences long-term sleeping issues lasting over six months. This problem is more prevalent in the Māori population at 19.1% compared to non-Māori at 8.9%. General practitioners (GPs) are responsible for diagnosing and treating insomnia, but there is no standardized national approach to doing so in New Zealand.
Insomnia has negative effects on a person’s physical and mental health and can increase morbidity and mortality rates. It has been linked to poor work performance, mental health disorders, accidents, high blood pressure, gastrointestinal disorders, diabetes, strokes and heart disease. Moreover, clinical studies have demonstrated that insomnia can impact a person’s ability to concentrate, cause daytime fatigue and the need for naps, lead to forgetfulness and increase the risk of accidents or falls. Despite its high prevalence and significant consequences, insomnia is often poorly evaluated and treated.

Blood Pressure
The proper functioning of the body relies on the circulation of blood which is vital. Through blood, nutrients and oxygen are distributed to all body parts. Maintaining a steady flow of blood from the heart to the brain and toes is crucial, and blood flow pressure is mediated by neurons in the medulla oblongata and nitric-producing bacteria in the mouth. In order to maintaining optimal health, the body must achieve precise coordination between the heart, blood vessels and kidneys under the supervision of the brain. This coordination is crucial to regulating blood pressure, which refers to the force exerted by blood on the walls of blood vessels, resulting from the heart’s rhythmic contractions that propel a constant volume of blood through a closed system. The primary factors influencing blood pressure are the inputs from hypothalamus to the Amygdala and spinal cord by affecting the cardiac output met by the peripheral resistance.
The balance of our body’s systems affects the circulation, which the neurohormonal system influences. The body responds to various stressors, including physical activity and mental health which can cause blood pressure to fluctuate throughout the day. To accurately measure blood pressure levels, it is necessary to consider both systolic pressure (during heart beats) and diastolic pressure (between heart beats) in the arteries. A GP will typically establish a baseline for an adult patient by conducting monthly tests over three months.

If high blood pressure is left unaddressed, prolonged hypertension can lead to serious physical health problems, including strokes, heart arrhythmias or heart failure, heart attacks, kidney, and eye damage.
Why Massage Therapy?
Today, massage therapy (MT) is commonly regarded as a therapeutic tool. It combines hands-on massage with self-care activities and health management to optimize treatment outcomes. Numerous evidence-based studies have shown that massage can reduce muscle tension, as reported by the individual and objectively measured through electromyographic testing. Additionally, MT can improve joint mobility, inflammation recovery, sleep mechanisms, breathing, and heart rate regulation. It has also been found to alleviate pain associated with musculoskeletal issues, tension headaches, migraines, pregnancy and cancer discomfort, depression, and anxiety. Furthermore, massage therapy can aid in pain management for conditions such as arthritis, fibromyalgia, multiple sclerosis, Parkinson’s disease, and dementia. It also improves pathophysiological dysfunction in diabetes and gastrointestinal disorders.
Massage therapy (MT) can profoundly impact the human body’s pathophysiology. It does this by eliciting neuromechanical responses that promote restoring the body’s homeostasis systems, resulting in a sense of relaxation, tranquility, and improved sleep. The effects of massage on the skin and the layers of fascia, muscle, and connective tissue are made possible by stimulating various receptors responsible for touch, heat, pressure, vibrations, and pain. This stimulation enhances the activity of the vagus nerve and the function of the autonomic nervous system, ultimately sending signals to the central nervous system (the brain and spinal cord), resulting in a range of physiological benefits.
As MT can influence the autonomic nervous system, which is responsible for maintaining homeostasis by regulating the activities of the viscera, blood vessels, and secretory glands in response to external stimuli. It helps to control the release of stress hormones by: (1) reducing cortisol, adrenaline, and noradrenaline; (2) regulating metabolism to enable the body to utilize other hormones like insulin, increasing dopamine, serotonin, and melatonin levels, and releasing endorphins; (3) improving microcirculation and blood flow to peripheral nerves. As a result, the mechanical stimulus from massage can induce a parasympathetic state, leading to the body’s regeneration and restoration of homeostatic balance.
Swedish Massage
Swedish massage is a very popular form of massage therapy that has been shown to alleviate both physical and mental health issues, benefiting individuals and the healthcare system as a whole. The treatment was created by Per Henrik Ling, a Swedish doctor, gymnast, and teacher in the 1800s. He called it the Swedish Movement Cure. Ling’s approach combined medical gymnastics and massage techniques, which served as a foundation for modern Swedish massage. This massage method utilizes gentle strokes, kneading, and striking movements with hands, forearms, and elbows on the body. Swedish massage uses light or deep gliding strokes, known as effleurage, to warm up superficial muscle areas and improve blood and lymph flow. Depending on the depth and direction of pressure applied, different functions can be served. Friction and stripping techniques are designed to lengthen muscles, while kneading and petrissage techniques relax muscle tension. Lastly, percussive movements like tapping, cupping, and hacking are used to stimulate nerves and remove mucus build-up within the lungs.
It is essential to maintain the balance of physiological processes for overall health and well-being. Lack of sleep (insomnia) can have negative effects on physical and mental health, leading to accidents, illnesses, and a lower quality of life. Insomnia disrupts the maintenance-repair stage, affecting neurohormonal processes. The medical field recommends a minimum of 7 hours of sleep for optimal cognitive and behavioural performance. Although general practitioners (GPs) in New Zealand are responsible for diagnosing and treating insomnia, there is no standardized national approach to doing so. Studies have shown that getting a massage can improve the quality and duration of sleep by promoting relaxation and improving overall well-being. However, it’s still unclear how many massages or what types of massages are needed to alleviate sleep issues. This case series study aims to determine if Swedish massage is effective enough for individuals to seek out on their own to help manage or alleviate their insomnia symptoms.
How I conducted the study
The three participants received Swedish massage treatment sessions lasting approximately 60 minutes for eight weeks. They completed the Sleep Quality Scale (SQS) questionnaire before and after the fourth and eighth massage treatments, as well as four weeks after the eighth treatment. In addition, their blood pressure was measured before each treatment session (initial, fourth, eighth, and post-four weekly), and they provided a subjective sleep score on a scale from 1 to 10 at the same intervals.
Study Design
The present case series study utilized a multi-method (mixed-method) approach, combining quantitative and qualitative data collection methods. This approach aims to offer a comprehensive understanding of the perspectives and beliefs of the study participants, as well as to use various outcome-measuring tools. The quantitative method involved using specific questionnaires (sleep quality scale and sleep score) and biological measurements (blood pressure). All these forms of data can be statistically analyzed.
Outcome Measuring Tools
The Sleep Quality Scale (SQS) is a tool designed to measure the quality of sleep. This scale evaluates six domains of sleep quality: daytime symptoms, restoration after sleep, problems initiating and maintaining sleep, difficulty waking, and sleep satisfaction. The SQS is a self-reporting questionnaire that takes 5 to 10 minutes to complete and consists of 28 questions. Respondents use a four-point Likert-type scale to indicate how frequently they exhibited certain sleep behaviours (0 = “few,” 1 = “sometimes,” 2 = “often,” and 3 = “almost always”). Total scores can range from 0 to 84, with higher scores indicating more acute sleep problems.
Blood pressure measurement was taken by a Sanitas SMB 18 sphygmomanometer, which is known for its high reliability and is recognized by the European Society of Hypertension and the German Hypertension Society. Readings were taken before the first, fourth, and eighth massage treatments as well as after the weekly treatments to observe any potential changes.
A subjective sleep score, that assess a participant’s sleeping habits. The score evaluates subjective sleep quality on a scale of 1 to 10. A score of 1-2 indicates poor to no sleep, 3-5 indicates disruptive sleep with difficulty returning to sleep, 6-8 indicates waking up but being able to easily fall asleep, and 9-10 indicates sound sleep throughout the night with feelings of restfulness upon waking. The sleep score offers insight into how an individual felt about their previous night’s sleep and whether they experience consistent sleep or struggled to fall asleep.
Participants’ Information
Two adult females aged between 29 and 65 years old and one adult male aged 43. Out of the two participants who took sleep medication, only one found it helpful, while the other stopped taking it. The remaining participant refused all prescribed medication. Additionally, all participants had issues with high blood pressure, struggled to fall asleep, and experienced broken sleep for over three years.
Case A
A 29-year-old female working as a senior IT engineer was diagnosed with stage 2 hypertension and insomnia three years ago and was prescribed blood pressure and sleep medication, which she has since discontinued due to perceived lack of efficacy. She used lifestyle changes (weight loss) to control her blood pressure instead of prescribed medication, a decision through her own research. In December 2022, she underwent surgery, she was experiencing another significant life change by separating from her long-term partner of seven years and moving into a new residence nine months ago.
Case B
A 69-year-old female, working as an event planner, who underwent double bypass heart surgery eight years ago and has been diagnosed recently with a 95% blockage in an artery, necessitating another surgery this year. Her cardiologist also diagnosed her with chronic insomnia in 2015 caused by pain. She takes medication to help her sleep but still experiences difficulties. She experiences low blood pressure that can cause dizziness and fainting at times. Her daughter nearly died from a sepsis infection eight weeks before this study.
Case C
In 2022, a 43-year-old male truck driver had learnt he had high blood pressure and chronic insomnia. Although he declined medication, he has modified his lifestyle to enhance his well-being. He recently came back to New Zealand after residing in the United Kingdom for two decades, and he is at present undergoing a divorce which began 6 months ago.
Massage Intervention
| Techniques | Description | Tissue | Duration | Reasoning |
| Effleurage | Gliding or sliding movement of hand/s in smooth continuous motion. | Legs, Erector Spinae Latissimus Dorsi, Trapezius. | 2-3 minutes on the back approx. 5 to 8 minutes | To stimulate parasympathetic nervous system and warm up the muscles, enhance venous return. |
| Petrissage or Kneading | Lifting, wringing, or squeezing in a kneading motion, or pressing and rolling of tissues under and between hands. | Deltoids Rhomboids, Upper trapezius, Levator scapulae, Supraspinatus, Quadratus Lumborum Hamstrings, Adductors (legs), Gastrocnemius, Soleus. | 1-2 minutes Upper back and neck and muscles around the scapulars 10-12 minutes Upper and lower leg total 8 minutes. | Mobilize deeper muscle tissue or the skin and subcutaneous tissue. To increase local circulation and help venous return. Mobilize deeper muscle tissue or the skin and subcutaneous tissue. To increase local circulation and help venous return. |
| Friction circles | Accurately delivered penetrating pressure applied through the fingertips. | Rhomboids, Upper trapezius, Levator scapulae, Supraspinatus, Quadratus lumborum | Upper and Lower Back – 8-10 minutes. | Treat muscle spasms or break up adhesions between muscles or from any old injuries. |
| Myofascial Release | Hands sink within the desired muscle or subcutaneous tissues and apply traction pressure. | Erector spinae Hamstrings Gastrocnemius | 1-minute hold 1-minute hold 1-minute hold | To release adhesions within the muscle or old injuries. To increase blood and lymph circulation return. To elicit a relaxation reflex response within the muscles. |
| Tapotement | Hand striking the tissue at fairly rapid rate. | All over the thoracic excluding the scapular. | 1-2 minutes | Stimulate tissues by direct mechanical force and to break up possible lung mucus. |
RESULTS
The graphs below are the data collected from the outcomes measuring tools used as well as the below graph showing average of hours slept through the 13-week period as I had gathered data on sleeping hours average for each participant a week prior to the start of the study.

The Outcome Measuring Tools results.
The Sleep Quality Scale
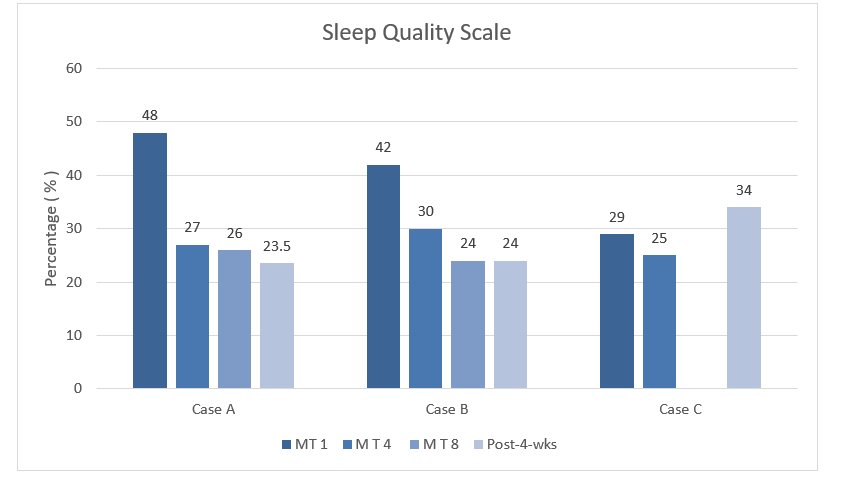
The initial Sleep Quality Scale (SQS) questionnaire in the above graph, revealed that all participants had difficulty staying asleep and desired more sleep almost every day. Over time, their desire for more sleep decreased to once or twice a week, compared to daily. After a month of no massages (post four weekly) the desire for sleep had risen again to often (3-5 times a week) throughout the week. All participants had sleep scores below 50 points, indicating that they did not reach the acute problematic stage (70) of insomnia.
The Subjective Sleep Scores

The Subjective Sleep Score is participants data around how they felt about the previous night’s sleep prior to their massage treatment. Please note the subjective sleep score ranges from 1 to 10: 1-2 for poor to no sleep, 3-5 for disrupted sleep, 6-8 for waking up but able to fall back asleep, and 9-10 for sound sleep throughout the night.
In Case A, between the third and fourth massage treatments, the individual’s partner experienced ill health and the related stress caused their sleep quality score to fluctuate. However, overall, they improved by 1.5 points. The highest score of 8/10 was experienced at the last massage treatment, indicating that they were able to get back to sleep easily once woken. There was an overall 7.6% improvement within the 12-week period.
Case B saw a significant 112% improvement, with the individual going from a score of 4 indicating broken sleep to a score of 8.5/10 of being able to get back to sleep and almost sleeping throughout the night at the eighth massage treatment. There was a 62.5% overall improvement within the 12-week time frame.
In Case C, the individual’s sleep quality varied, but there was an overall 50% improvement of 3 points, going from a score of 6 indicating broken sleep to a score of 9, indicating sleeping throughout the night and feeling rested in the morning at the eighth massage treatment. The case finished with a score of 7/10 at the post-4-weekly, thus making a 16.6% improvement overall.
Blood Pressure
The blood pressure baselines

The blood pressure readings for the three participants varied. In Case A, the scores fluctuated but still improved from the initial baseline of 141/90 to 135/96, with a decrease of 6 points in the systolic and increase of 6 points on the diastolic readings.
Case B, on the other hand, experienced an increase in blood pressure from 107/90 to 132/96 before eventually dropping to 106/74 without any side effects of light-headedness. This resulted in a 1-point overall drop in their baseline systolic readings and a 16-point drop in diastolic readings.
In Case C, there was a continuous decrease from 175/120 to 150/113, with a 25-point drop in systolic and a 7-point decrease in diastolic readings.
Participants Perspective
Participants reported a positive experience from monitoring their sleep habits. The MT was especially helpful, with participants feeling better the night of the massage and in the following evenings. One participant, who previously only got 1-3 hours of sleep per night and would often ‘crash,’ is now getting double the amount of sleep per night.
Conclusion
In summary, the research findings reveal that massage therapy offers many benefits to enhance sleep quality. Massage therapy amplifies the body’s natural restorative processes, helping to achieve longer and more restful sleep cycles while improving cognitive and behavioral performance in both professional and social environments. Additionally, it has been shown to have positive effects on blood pressure, which is crucial for maintaining good health and wellness.
However, the study is limited by its sample size, which impacts the representativeness of the findings. Therefore, further research with a larger sample size is necessary. In conclusion, these findings suggest that massage therapy is a safe and effective solution for improving sleep quality and enhancing overall health.